Epidural Steroid Injection (ESI)
Overview
An epidural steroid injection (ESI) is a minimally invasive procedure that can help relieve neck, arm, back, and leg pain caused by inflamed spinal nerves. ESI may be performed to relieve pain caused by spinal stenosis, spondylolysis, or disc herniation. Medicines are delivered to the spinal nerve through the epidural space, the area between the protective covering of the spinal cord and vertebrae. The effects of ESI tend to be temporary. Pain relief may last for several days or even years. The goal is to reduce pain so that you may resume normal activities and a physical therapy program.
What is an epidural steroid injection (ESI)?
An epidural steroid injection includes both a long-lasting corticosteroid (e.g., triamcinolone, betamethasone) and an anesthetic numbing agent (e.g., lidocaine, bupivacaine). The drugs are delivered into the epidural space of the spine, which is the area between the protective covering (dura) of the spinal cord and the bony vertebrae. This area is filled with fat and small blood vessels.
Epidural space
The epidural space, which lies between the dura mater and the bony vertebra, is filled with fat and blood vessels. The dural sac surrounds the spinal cord and nerve roots and contains cerebrospinal fluid.
Corticosteroid injections can reduce inflammation and can be effective when delivered directly into the painful area. Unfortunately, the injection does not make a herniated disc smaller; it only works on the spinal nerves. The pain relief can last from days to years, allowing you to improve your spinal condition with physical therapy and an exercise program.
Who is a candidate?
Patients with pain in the neck, arm, low back, or leg (sciatica) may benefit from ESI. Specifically, those with the following conditions:
Spinal stenosis: A narrowing of the spinal canal and nerve root canal can cause back and leg pain, especially when walking.
Spondylolysis: A weakness or fracture between the upper and lower facets of a vertebra. If the vertebra slips forward (spondylolisthesis), it can compress the nerve roots causing pain.
Herniated disc: The gel-like material within the disc can bulge or rupture through a weak area in the surrounding wall (annulus). Irritation, pain, and swelling occur when this material squeezes out and comes in contact with a spinal nerve.
Degenerative disc: A breakdown or aging of the intervertebral disc causing collapse of the disc space, tears in the annulus, and growth of bone spurs.
Sciatica: Pain that courses along the sciatic nerve in the buttocks and down the legs. It is usually caused by compression of the 5th lumbar or 1st sacral spinal nerve.
ESI has proven helpful for some patients in the treatment of the above painful inflammatory conditions. ESI can also help determine whether surgery might be beneficial for pain associated with a herniated disc. When symptoms interfere with rehabilitative exercises, epidurals can ease the pain enough so that patients can continue their physical therapy.
ESI should NOT be performed on people who have an infection, are pregnant, or have bleeding problems. It may slightly elevate the blood sugar levels in patients with diabetes, typically for less than 24 hours. It may also temporarily elevate blood pressure.
Who performs the procedure?
The types of physicians who administer epidural steroid injections include physiatrists (PM&R), anesthesiologists, radiologists, neurologists, and surgeons.
What happens before treatment?
The doctor who will perform the injection reviews your medical history and previous imaging studies to plan the best approach for the injections. Be prepared to ask any questions you may have at this appointment.
Patients who take take blood thinner medication (Coumadin, Heparin, Plavix, Ticlid, Fragmin, Orgaran, Lovenox, Innohep, high-dose aspirin) may need to stop taking it 3 to 5 days before the ESI. Discuss any medications with your doctors, including the one who prescribed them and the doctor who will perform the injection. If you take Coumadin, a blood draw will be done at least 2 hours prior to the procedure to test your blood clotting (PT-INR test).
If you think you may be pregnant or are trying to get pregnant, please tell the doctor. Fluoroscopy x-rays used during the procedure may be harmful to the fetus.
Day of the procedure
Plan to arrive 15 minutes before your scheduled appointment time.
We recommended that you have something light to eat prior to the appointment.
Make arrangements to have someone drive you to and from the office or outpatient center the day of the injection.
What happens during treatment?
The goal is to inject the medication as close to the pain site as possible, using either a translaminar or transforaminal injection. The right type of injection depends on your condition and which procedure will likely produce the best results and the least discomfort or side effects. Studies have shown that use of fluoroscopy (X-ray) to guide the needle into the epidural space is more effective than when the ESI is performed without fluoroscopy. The procedure usually takes 15-30 minutes and is followed by a recovery period.
Step 1: Prepare the patient
Patients can remain awake for the entire process. Sedatives can be given to help lessen anxiety. Lying face down on the table, the patient receives a local anesthetic, which will numb the skin before the injection is given. If IV sedation is used, blood pressure, heart rate and breathing are monitored during the procedure.
Step 2: Insert the needle
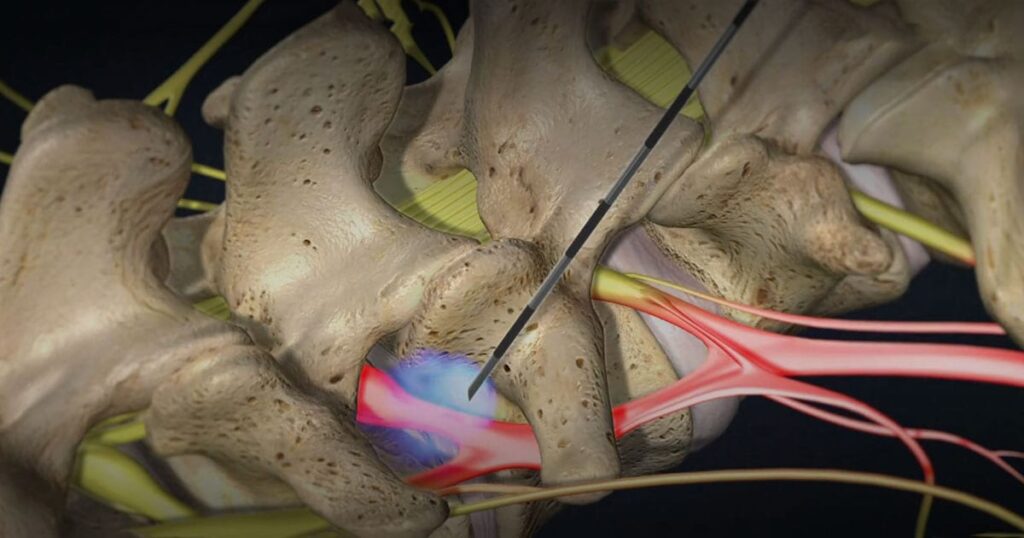
With the aid of a fluoroscope (a special X-ray), the doctor directs a hollow needle through the skin and between the bony vertebrae into the epidural space. Fluoroscopy allows the doctor to watch the needle in real-time on the fluoroscope monitor, thus ensuring that the steroid medication is delivered as close to the inflamed nerve root as possible. Some discomfort occurs but patients typically feel more pressure than pain.
There are three ways to deliver epidural steroid injections: translaminar, transforaminal, or caudal approaches. The best method depends on the location and source of pain.
Translaminar ESI. The needle is placed between the lamina of two vertebrae directly from the middle of the back. Also called interlaminar, this method accesses the large epidural space overlying the spinal cord. Medication is delivered to the nerve roots on both the right and left sides of the inflamed area at the same time.
Translaminar injection
Translaminar injection (cross-section view of vertebral column) shows the needle inserted into the epidural space behind the spinal cord to deliver steroid medication to the inflamed nerve root.
Transforaminal ESI. The needle is placed to the side of the vertebra in the neural foramen, just above the opening for the nerve root and outside the epidural space. Use of a contrast dye helps to confirm where the medication will flow when injected. This method treats one side at a time. It is preferred for patients who have undergone a previous spine surgery because it avoids any residual scars, bone grafts, metal rods, and screws.
Transforaminal injection
Transforaminal injection (side view of vertebral column) shows the needle placed in the neural foramen to deliver steroid medication to the inflamed nerve root.
Step 3: inject the medication
When the needle is in place, the local anesthetic and steroid medication are delivered to the epidural space. The needle is then removed.
What happens after treatment?
Most patients can walk around immediately after the procedure. After being monitored for a short time, you usually can leave the office or suite. Someone must drive you home.
Typically patients resume full activity the next day. Soreness around the injection site may be relieved by using ice and taking a mild analgesic (Tylenol).
The doctor’s office may want to follow up 7 to 10 days after the procedure to ask about your symptoms and the level of pain relief obtained. You may want to record your levels of pain during the next couple of weeks in a diary. For patients whose pain is greatly improved, further procedures or surgery may be unnecessary. For patients whose pain is not relieved, the next steps in their care are discussed with their physicians.
What are the results?
Many patients experience some pain relief benefits from ESI [1,2]. For those who experience only mild pain relief, one to two more injections may be performed, usually in 2-week intervals, to achieve full effect. The benefits of ESI tend to be temporary. Duration of pain relief varies, lasting for weeks or years. More importantly, timing of injections should coincide with the start of a physical therapy and/or home exercise program to strengthen the back muscles and prevent future pain episodes.
What are the risks?
With few risks, ESI is considered an appropriate nonsurgical treatment for some patients. The potential risks associated with inserting the needle include spinal headache from a dural puncture, bleeding, infection, allergic reaction, and nerve damage / paralysis (rare). Corticosteroid side effects may cause weight gain, water retention, flushing (hot flashes), mood swings or insomnia, and elevated blood sugar levels in people with diabetes. Any numbness or mild muscle weakness usually resolves within 8 hours in the affected arm or leg (similar to the facial numbness experienced after dental work). Patients who are being treated for chronic conditions (e.g., heart disease, diabetes, rheumatoid arthritis) or those who cannot temporarily discontinue anti-clotting medications should consult their personal physician for a risk assessment.